Many people would suppose that medical devices are subject to the same stringent approval and inspection processes as medicines. But they would be wrong.
When it comes to devices such as hip joints and breast implants, a manufacturer is not required to win a licence based on evidence of safety and efficacy from clinical trials. Instead, they must get a CE mark which certifies the product reaches a certain European quality standard. It is the same mark that a Chinese toy company, for example, would have to obtain to sell yo-yos in Europe.
Medical devices are an enormous global industry, with 18,000 companies in Europe alone. As production has become cheaper elsewhere, so companies have moved.
The world leader in breast implants is the US company Allergan, which used to make them in Ireland. In the past couple of years, it has moved to Costa Rica. Its products have a CE mark, which means they have been quality-approved by a "notified body" in Europe. Inspectors, it says, come from all over the world to ensure standards remain high.
This is because EU directives lay out what commercial companies have to do to get the CE mark, wherever in the world they are based. "It is the same thing with toys. All products must have a CE mark," said Frederic Vincent, EU spokesman on health and consumer policy. "Some 80% of toys are produced in China. Manufacturing plants in China have all the papers needed."
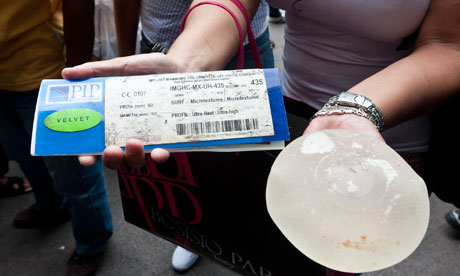
Regulating the number and variety of medical devices is a huge job. The CE mark assessment must be done by one of the EU's accredited "notified bodies", but it does not have to be in the country of the manufacturer – the company gets to choose. PIP (Poly Implant Prothèse), the French manufacturer of the sub-standard breast implants that have caused the scandal, elected to apply not to a French notified body, but to one in Germany, called TÜV Rheinland.
The assessment is necessarily much tougher for breast implants, which have been reclassified in recent years as class III medical devices, than for bandages, for example, which are class I. PIP would have had to submit a dossier of evidence that its products were of high quality and its factory processes would have been examined.
The trouble began after PIP had obtained its CE mark. TÜV Rheinland, which has a good reputation in Germany, did send in inspectors on occasion. But PIP knew they were coming. A defiant Jean Claude Mas, the owner of the company, admits he was buying cheap industrial-grade silicone to fill the implants, costing €5 a litre, instead of medical-grade which cost €35.
"TÜV would announce its visits 10 days beforehand," he told French journalists. "That was the routine. I would give the order to hide all the documents regarding the non-authorised PIP gel and as far as the containers were concerned, the staff would organise themselves to make them disappear."
Thierry Brinon, technical director of the company, who said he was recruited from "a small ad", told investigators that "for as long as organisations give us systematic notice of inspection, any kind of malpractice can be hidden".
That was fraud, points out Vincent. Nonetheless, there are now questions over the safety of the European regulatory system. If unannounced inspections are not carried out, then the only warning of problems with the devices is when they go wrong. But it could take a long time for the authorities to realise there is a serious problem.
Doctors and surgeons are supposed to report adverse events – side-effects or health issues they suspect are caused by the devices – to the company and to the regulator in their own country. A company such as PIP may take no notice, even though it is under an obligation to report serious problems. The rupture of a breast implant is not considered serious enough to be reportable, because it can be caused by an accident.
Problems in the UK should be reported to the regulator, the Medicines and Healthcare Products Regulatory Authority (MHRA). Although the MHRA licenses drugs, it has no responsibility for approving medical devices. All it can do, if it has evidence of issues, is send out a letter warning doctors.
That happened in April 2005. The MHRA had concerns about the safety of breast implants made of polyurethane foam and filled with silicone. They were introduced in the 1970s and withdrawn worldwide in 1991 because of fears the polyurethane coating could break down, releasing carcinogens.
The manufacturer, Polytech Silimed Europe, presented the MHRA with new safety data, but its experts said they could not be sure the improvements outweighed "the remote but unquantifiable carcinogenic risk". However, the MHRA could not stop the company selling its CE-marked implants in the UK. "As the implants are CE-marked medical devices, the MHRA accepts that they can legitimately be placed on the UK market, provided users and potential recipients are appropriately informed about their risks and benefits," it said in the 2005 letter.
It takes a substantial weight of evidence of harm – which has to come from all over Europe – to get an implant banned. If there are a few cases in the UK, a handful in France and some in Italy, the regulators in each country would have to talk to the others for the problem to be taken seriously. If the company is behaving ethically, it will be the first to know because it will get complaints from everywhere and can alert the rest of the world. But a company like PIP can sit on the evidence.
Breast implants have a long history of anxieties and recalls, followed by attempts by women to get legal redress and compensation. In 2000, hydrogel implants manufactured by PIP and given to 4,000 women since 1994 were voluntarily withdrawn. But there were warning signs around PIP even at that time. The MHRA stated that its review "has identified that the manufacturer's biological safety assessment of this product in inadequate, due to the lack of long-term toxicity data or clinical follow-up, together with methodological flaws in some of the pre-clinical tests".
Women sued and the UK courts awarded compensation, but PIP's insurers refused to pay up. Mark Harvey of Hugh James, the Cardiff-based solicitors, who ran claims then and has 300 women on his books over the latest PIP implant scandal, maintains the MHRA is to blame. "PIP has been able to come back into this country with a defective product and walk away again," Harvey said.
He also said the agency had not been sufficiently alert and responsive in the past year or more since the implants had been banned. "I do not believe the MHRA's reaction to date has been satisfactory; it is unbelievable the MHRA has not ensured that it was involved with the consultations in France about a product that affects such a large amount of women in this country.
"I am and have been very critical of its role throughout the history of this product. This stems from allowing this company to sell these implants in the UK in the first place, its refusal to respond when I alerted it to the problems, its refusal to meet with any of my clients to discuss their concerns and now this latest health concern."
There have been other warnings that tougher regulation is needed. Thousands of patients in the UK and many more around the world are facing operations to replace an artificial hip joint which was found to cause great pain and deposit toxic metal in the blood. The joint, made by DePuy, which is part of the huge Johnson & Johnson group, was made entirely of metal, instead of metal and plastic. The MHRA issued a recall in September last year.
Doctors and surgeons have to play their part in ensuring the safety of devices. There have been allegations that the relationships between some doctors and employees of the manufacturers are too cosy. "The device companies have tried to have good relationships with surgeons for decades," said Alison Dennis, a partner at law firm Field Fisher Waterhouse who has long worked with the industry. "That is how devices are developed." Surgeons advise companies and test out their products but sometimes the relationships, built up over years, go beyond the professional, she said.
The European-wide trade body, Eucomed, set out an ethical code in 2008, requiring members not to meet doctors unless for work and not to offer rounds of golf or visits to the spa. The major companies, she said, had taken the code on board, helped by major fines for malpractice in the US.
Many think the system is tougher in the US than in Europe. Britain's only breast implant manufacturer, Nagor, which has an exemplary record, is still struggling through the regulatory hoops to win approval. Regulation is through the centralised Food and Drug Administration, which also licenses drugs.

